Clinical Exercise: Lateral Orbital Canthotomy
Scenario:
Working late in the emergency room a patient presents with visible bruising around the left orbit. The patient reports that they fell and their eye hit the corner of a table. The patient further indicates that they were able to see through the affected eye a few minutes ago, but vision in that eye has deteriorated and is no longer present. The patient is also unable to move that eye.
Diagnosis:
You recognize that acute loss of vision from that eye is a time-critical emergency procedure and examine the patient's eye with a bright light. The patient reports being unable to see the light from the affected eye and you observe no pupillary reflexes. The eyeball appears pressed forwards and there is considerable soft tissue edema surrounding the eyeball. You suspect a retrobulbar hemorrhage resulting in an orbital compartment syndrome and recognize the need to perform an immediate lateral orbital canthotomy.
Mechanism:
Due to the eyelid structure the orbit is a closed structure with limited anterior displacement of the eyeball. Retrobulbar hemorrhage raises the pressure in the orbital cavity. This elevated orbital pressure reaches the point that the ophthalmic artery is compressed compromising blood supply to the orbit. This results in hypoxia to the orbit tissues and cessation of nerve/muscle function. Unless the pressure is released, allowing blood to perfuse back into the tissues, irreversible vision loss will occur in as little as 90-120min. In patients with facial fractures ~25% will have serious to blinding severity of orbital compartment syndrome requiring intervention.
Treatment (perform these steps on your donor in a mock-procedure):
1) Inject a local anesthesic into the lateral region of the eyelid, the lateral canthus (perform a mock injection using a probe as a substitute for needle positioning).
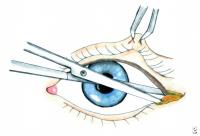
2) Using a hemostat or forceps clamp the skin at the orbital rim firmly.
One arm of forceps is positioned on the inside of the eyelid
all the way to the orbital rim. Position the other arm of the forceps outside
the eyelid so that the skin is 'crimped' between the arms. This crimp achieves hemostasis in the living and serves
as a location for incision (in the living you hold the clamp for 30-60 seconds).
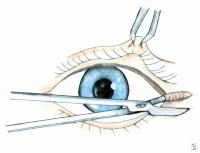
3) Use forceps to pick up the skin at the lateral orbit.
4) Use scissors to make a 1-2cm incision beginning at the lateral corner of the eye and extending laterally to the orbital rim.
Scenario (addendum):
In the patient, you observe that this did not relieve sufficient pressure from the hemorrhage and you decide to extend the canthotomy procedure into a cantholysis.
Treatment (continued):
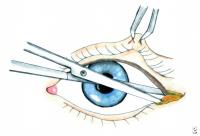
6) Grip the lower eyelid and pull firmly inferiorly.
 This tenses the lateral canthus tendon and allow it to be visualized (this is a Y
shape tendon attaching to the orbit with a Y-arm to each of the eyelids). The
tendon may not be distinctly visible, but the 'stretched' part of tissue will
house the tendon.
This tenses the lateral canthus tendon and allow it to be visualized (this is a Y
shape tendon attaching to the orbit with a Y-arm to each of the eyelids). The
tendon may not be distinctly visible, but the 'stretched' part of tissue will
house the tendon.
7) Using scissors (or a scalpel if the donor tissue is overly firm), transect the lower 'arm' of the lateral canthus tendon.
8) The inferior cantholysis was still insufficient to relieve the pressure and you decide to transect the superior arm of the lateral canthus tendon as well.
9) Repeat the cantholysis steps only pulling the upper eyelid superiorly to stretch and observe the superior arm of the lateral canthus tendon.
Upon restoration of blood flow and management of the initial injury, you would repair the severed structures with suture. As we will be removing the eyelid in later steps leave the canthotomy/cantholysis open.
Outcome:
With the performance of the lateral orbital canthotomy and cantholysis you observe the eyeball bulging further from the orbit. The patient reports they are starting to see again and you observe pupillary responses to bright light returning.